
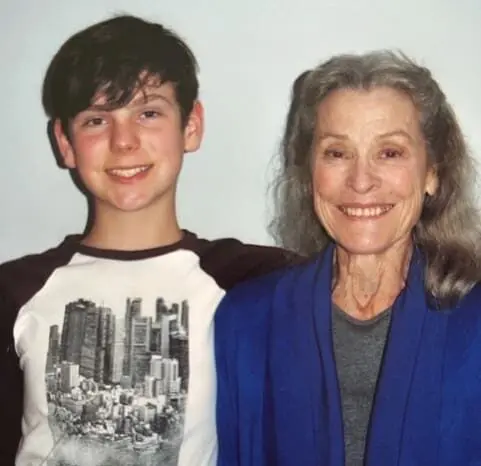
Yvonne was asymptomatic and shocked to learn she may have the early stages of aggressive cancer.
Yvonne, 77 years old, had experienced good health all her life. She had been suffering from a minor chest infection and booked an appointment with her local GP who referred her for a CT (computer tomography) scan for a more detailed image of her chest.
“The result came back that my lungs were clear,” said Yvonne, “but the scan revealed a cyst on my pancreas.”
Her GP said he didn’t like the look of the cyst and referred her to hepatobiliary and pancreatic surgeon Professor Jaswinder Samra at Royal North Shore Hospital (RNSH).
Yvonne went to Professor Samra’s room thinking he might give her some medicine to treat the cyst or at worst a small operation.
“In Yvonne’s case, she had an intraductal papillary neoplasm (IPN) measuring 34mm located at the junction of the duodenum and pancreas,” said Professor Samra. “While it was currently benign, if left untreated she ran the risk of it developing into pancreatic cancer and a 12% survival rate within five years.”
Yvonne remembered Professor Samra asking “what will you be doing in five years’ time?” She thought to herself “why did he want to know that?” At that point Professor Samra told her that if she didn’t have the IPN removed, she had a 44% chance of being alive in five years’ time.
Yvonne was surprised at the diagnosis, as she was asymptomatic, and she had not realised that the IPN has the potential to become malignant.
More than 4,500 Australians will be diagnosed with pancreatic cancer in 2023. The average age at diagnosis is 72 years old. Pancreatic cancer is the eighth most diagnosed cancer in Australia, with an estimated one in 70 people diagnosed by the time they are 85.
Early-stage pancreatic cancer rarely causes symptoms, so it is typically diagnosed late, leading to poor prognosis. It is only once the cancer is large enough to affect nearby organs or has spread, that symptoms start to appear.
“Patients with pancreatic pathology (cancer or precancerous lesions) are best looked after by a multidisciplinary team within a high volume unit. Patients need to be informed and given up-to-date information,” said Prof Samra.
In discussing the surgery with Yvonne, Professor Samra drew a diagram and discussed with her what organs had to be removed and relocated in a procedure called a pancreaticoduodenectomy.
Also known as a Whipple, named after American surgeon Allen Oldfather Whipple, it is a major complex operation as the pancreas is located deep inside the abdomen next to major blood vessels. In Yvonne’s case, part of her pancreas, duodenum, bile duct along with her gallbladder were removed, reconstructed and reconnected to her stomach and small intestine.
“It was quite a big plumbing job,” said Yvonne.

The surgery at RNSH lasted for six hours, and Yvonne woke up in recovery feeling nauseous and having a very dry mouth. She recalls Vic, the nurse caring for her, was very cheerful and attentive and gave her some crushed ice.
Besides the IV (intravenous) tube in her arm for fluids, she had several drainage tubes in her abdomen which were uncomfortable and limited her movement, in addition to the 20 staples on her mid-line incision. She was allowed to eat soft foods which included yoghurt, jelly and juice.
Her stomach was numb for the first few days, and she experienced no pain. By the third day, Yvonne was able to walk and have a shower.
“The nurses were very good,” said Yvonne. “I was well looked after, and I couldn’t ask for more. Professor Samra was excellent, and he explained the operation very clearly.”
She was discharged from RNSH after 10 days and as part of her discharge plan, a nurse visited her daily to assess and dress her wounds and remove the staples.
The side effects Yvonne recalled were a slight burning sensation from acid reflux in addition to gaining 10kg in fluid. The drainage tubes had been removed in hospital, however the pancreatic juices continued to flow from the site of the incision and Yvonne was constantly changing her clothes every hour for a few days as they became saturated.
Yvonne continued to see Professor Samra annually for five years and she has received a clean bill of health. She is thankful that her GP sent her for a scan, and she was able to receive treatment early.
Pancreatic cancer can be a silent killer as it is usually not discovered until it is well advanced. To improve the prognosis of patients with pancreatic cancer, there is an urgent need for specific early detection and diagnosis tests.
Senior Cancer Research Fellow at The Kolling Institute, Dr Sumit Sahni is analysing plasma derived extracellular vesicles (EVs) which could serve as a valuable source of early detection biomarkers for pancreatic cancer and improve survival outcomes.
Working closely with Professor Samra, Dr Sahni’s aim is to research innovative approaches to develop minimally invasive and inexpensive tests for the early detection and diagnosis of pancreatic cancer.
If you would like to support pancreatic cancer research at the Kolling Institute, please make a donation here.
