
Baby Elijah was born prematurely via an emergency caesarean as he was at risk of being deprived of oxygen. While a normal birthweight is between 2500g and 4499g, Elijah weighed just 1323g.
Elijah’s parents, Calista and Paul, were overjoyed when they found out they were going to have a baby after only a few months of trying. Their joy was immediately cut short as on the same night Calista found out she was pregnant, she started to bleed. She consulted her GP who advised her that the chances of her miscarrying were high.
However, to their surprise, Calista didn’t miscarry. She sailed through her pregnancy until her 20-week scan revealed she had a short cervix, which meant she was at high risk for a premature birth. More concerning, when Calista was 22 weeks pregnant, her cervix dilated to three centimetres. To delay labour, her obstetrician performed a cervical cerclage or stitch at the neck of the cervix.
Calista was on strict bedrest at home and had weekly scans, but when she was 25 weeks pregnant, the scan showed her cervix had now dilated to nearly four centimetres.
Calista was booked in to give birth at a private hospital, however with the chance her baby would arrive within the next few days, she had to be immediately admitted to Royal North Shore Hospital (RNSH) which has the only local specialised Neonatal Intensive Care Unit (NICU).
“I can still remember the first day of admission when I heard the statistics of a baby born at 25 weeks. Staff informed us of the increased risk of special needs, the survival rates of a baby born prematurely at 25 weeks, and what kind of support a baby would need. We discussed the resuscitation support for our baby after the birth, that’s when the seriousness of the situation hit us.”
Calista recalls it was a surreal time, but she refused to allow herself to take on the stress of the situation. Instead, she celebrated every day that she was still pregnant as a blessing and answered prayer.
Professor Kluckow from the RNSH NICU team said they hoped to get the baby to 28 weeks as it would be a game changer in terms of the baby’s health and weight. At 25 weeks, Calista’s baby was estimated to weigh 750g.
At 28 weeks, Calista began to bleed heavily as her cervix continued dilating, tearing the cerclage. The night after her stitch was removed, Calista’s cervix continued to dilate, and her contractions started.
An emergency caesarean was performed as Elijah was at a high risk of being deprived of oxygen due to his breech position and umbilical cord presentation. As soon as he was born, he was immediately handed to Dr Eveline Staub, a neonatal intensive care physician.
“When he was born, anxiety and worry kicked in,” said Calista who explained up until this point she felt calm.
As new parents, they wanted to be informed of all possible scenarios, but all the information they were processing about Elijah’s health became overwhelming.
“That’s when Dr Staub stepped in,” said Calista. “She explained that Elijah was a good weight, and doing well, giving us much needed comfort and peace.”
Calista remembers that Dr Staub’s method of communication was filled with compassion and understanding.
Paul said that even though they felt they were in such a stressful scenario, they knew Elijah was in the best facility with excellent equipment and healthcare professionals available around the clock, and that brought them an enormous peace of mind.
They are extremely grateful for the compassionate nursing staff in NICU who provided all types of support in a difficult situation.

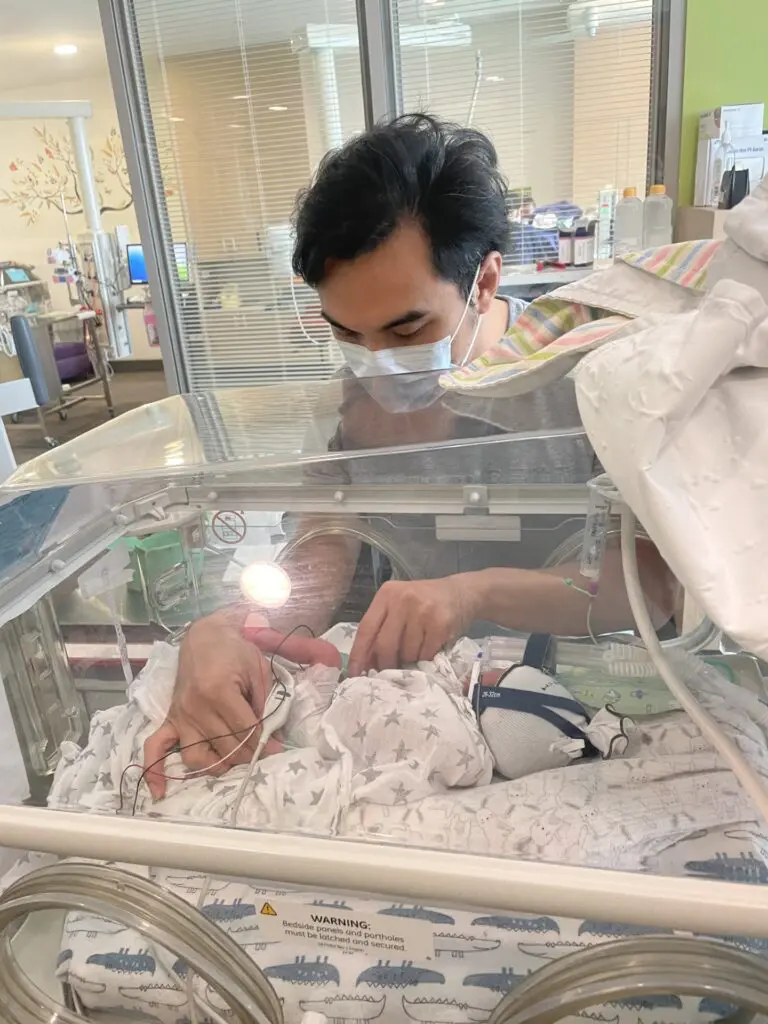

“I couldn’t recognise Elijah as the mask he was wearing for respiratory support was covering his face,” Paul said.
“The nurses did all they could to help us look at Elijah’s face. The nurses even took photos of Elijah’s feet for a Mother’s Day card, something we treasure to this day.”
Paul said it felt daunting handling such a tiny baby, but he was grateful the nurses encouraged him to be hands-on, giving him added confidence as a father.
Thankfully, Elijah didn’t suffer any health issues and was discharged after the family spent nearly 100 days in hospital.
During Elijah’s stay in hospital, his parents witnessed the dedication and professionalism of the healthcare staff first hand. Calista and Paul said they felt extremely supported as a family by the team of doctors and nurses which included allied healthcare staff.
“It takes a village to raise a child and we saw that village in a hospital setting,” said Calista. “The community of doctors, nurses and allied healthcare staff have been pivotal in Elijah’s health, growth and development.”
Elijah is now a thriving baby, full of energy and smiles. He is reaching all his milestones and growing well.
“Success stories like Elijah’s make me incredibly proud to be part of the NICU team at RNSH,” said Dr Staub. “It is our privilege to look after these precious children and also caring for the parents in these exceptional circumstances. I am delighted to see Elijah grow and thrive – congratulations to Calista and Paul on their wonderful job as parents.”
Calista and Paul want to share their story to give hope and comfort to others who are going through a similar difficult time.
Elijah was one of the 550 babies who were admitted to Neonatal Intensive Care and Special Care Unit at RNSH last year.
If you would like to support the care of pre-term babies in the Neonatal Intensive Care Unit at RNSH, please make a donation here.
